Occupational role in shaping infections
“In the past 30 years, Asia has been at the epicentre of 30 emerging infections”
-WHO, A brief guide to emerging infectious diseases and zoonoses
- Avian influenza
- Chikungunya
- Crimean-Congo haemorrhagic fever
- Dengue
- Zika
- Ebola virus disease
- Hantavirus
- Hand, foot and mouth disease
- Japanese encephalitis
- Nipah virus
- Novel human coronavirus
- Rabies
- Rift Valley fever
- Viral hepatitis
From the shape-shifting clutches of SARS and influenza virus to vector borne infections in form of Chikungunya and Zika.
Within the past two decades; the economic trends of progress, growth trends of population and epidemiological shifts in infections have all pointed to the East – Asia, in particular. All the three indicators of progress: booming economies, rising population and melding international boundaries have created biological ripples.
Jobs now require frequent transitions from one geography to another – from a senior IT executive to a daily wage labourer – biological context changes and its characteristics get carried over. An endemic infection outbreak of swine flu can now overarch and stretch modern medicine by the virtue of virulence and spread over with damning robustness and ruthless efficiency.
Occupational centres, occupation and trade remains central to this theme of how modern emerging infections are being shaped. As you read these lines, a business executive sick with influenza can travel via airports, local transit systems and cab rides creating an infectious trail for weakened immune systems to fight.
Similarly, the same executive at their workplace (attended by hundreds or different individuals) can effectively increase the chances of contracting an infection due to the set 8-9 hours spent together, daily. This is where we come in contact, interact and spend our working lives sitting closely to each other. The modern workplace is mostly local exhaust ventilation dependant environment. Closed, ventilated from single source without much exposure to best sanitizer in the world – sunlight. Or, in case of industrial workplace, a mix of stressful or sometimes even sterile work environments.
The takeaway from this premise is that our exposure times increase significantly while at office. The ventilation, cleanliness and personal hygiene routine can be easily overpowered by frequent contact with commonly used surfaces (washroom, office door handles or even coffee room utensils).
Office workplaces can mitigate the chances of becoming petri dishes of bubbling infections by some common disease control strategies:
- Soap, water, rinse and repeat at least 3 times a day.
- Local exhaust ventilation and AC maintenance and cleaning routine should be stricter, to avoid Sick Building Syndrome.
- Sick employees should be provided convenient time-off options (with work from home).
- Water cooler, coffee rooms and cafeteria should have a “double door” isolation – extra space between them and other office areas to mitigate contact spread of infection (though hand wash and regular cleaning can overcome physical challenges).
- Common surface contact accessories (computer mouse, keyboard, slide changers) should be cleaned periodically with alcohol wipes to ensure grime and dirt doesn’t harbour pathogens.
- Pest control means a thorough approach to not only control pest and zoonoses agents but create mitigation barriers that focus on becoming effective repellent.
There is a very strong case for why Asia has been at the centre of emerging infections, biological outbreaks and will suffer the most for at least next decade.
Climate change has driven tropical temperatures to scorching levels, deforestation has driven forest dwelling species closer to our villages and cities. This has increased our susceptibility to infectious agents – faster biological lifecycles of pathogens supported by better transmission rates and increase in population means that ‘virulence’ finds a better learning system to become more and more lethal each time it infects someone, more swiftly than in previous times. Frequent animal contact and ‘factory scale’ farming and animal husbandry adding fuel to this fire of disease transmission.
To grasp how average flu is changing and jumping hosts faster, better and with increased virulence, all find its progenitor in our human acts. Correcting the course would mean a better information and communication strategy for rich and poor alike with vaccine and medicine research focusing on preventive methodologies rather than a wait-and-watch approach.
Occupational areas where large number of individuals gather, and work should undertake proactive steps for ensuring hygiene, cleanliness and routine testing procedures. The organization not only owes it to the personnel but for the larger question, at play.
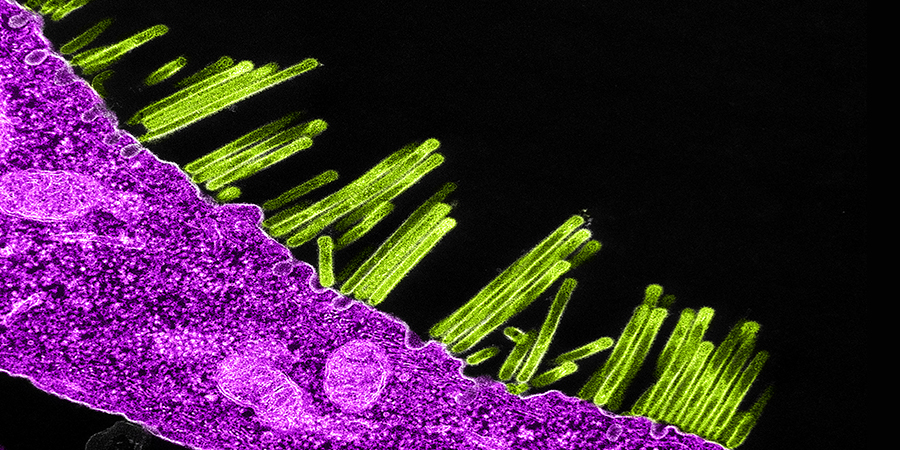
Image Credit: NIAID